CLARKSBURG — Cancer care and treatment is a continuously evolving field, and one that healthcare professionals in North Central West Virginia are passionate about.
Linda Carte, RN, MSN, AOCN, vice president of oncology at United Hospital Center, said the facility is making every effort to improve patients’ experiences with their treatment program.
“UHC is participating in a oncology care model, which is a group of activities that are put together for patients, with the ultimate goal of improving coordination of services to improve communication between all the members of the care team and ultimately improve outcomes for the patient,” Carte said. “The reason that we put all of these things together through this model is to try to decrease the risk of patients developing adverse events.”
Carte said “adverse events” could mean having to come back to the hospital or not having their side effects managed properly. She said that by using the new care model, different parts of the program work together to make the system better for the patient.
“We’re very proud to have been chosen to participate,” Carte said. “Only around 200 facilities across the country were chosen. We feel like we were chosen because we already had a lot of the pieces in place, such as electronic medical records that allow the doctor to see what’s going on with the patient no matter where they are, patient navigation and doctors being available 24 hours a day. There’s always room for improvement when it comes to cancer care, but this program provides an opportunity to make a difference in the care of a patient with cancer.”
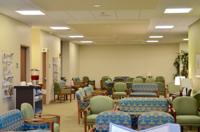
In addition to working to optimize its treatment programs, United Hospital Center has also worked to improve the physical layout of the Cecil B. Highland Jr. and Barbara B. Highland Cancer Center, finishing the last of the renovations in January.
“Treatments change all the time, so the length of treatment can be anywhere from 5 minutes to 10 hours with us, depending on what type of cancer the patient has,” Carte said. “What we found over the past couple of years is that we needed more space to provide the services that patients need. The remodeling has allowed us to combine the physicians’ offices into a pattern that makes sense for the patient. They walk in, then get their blood drawn. Then they get seen in the physician office and then they flow back to the treatment space. So the remodeling allowed for ease of the time that they spend in the cancer center.
“Prior to this, because we had two private physician offices, the areas weren’t connected very well,” Carte said. “Part of our responsibility is making sure that treatment days or physician appointment days are as easy as possible. We know that when patients are on treatment, their energy is not limitless, so we want to make sure that the energy they have, they can spend doing the things that they want to do. They shouldn’t be exhausted at the end of their treatment day, so we put together a layout that makes sense to the patient.”
Another level of care that United Hospital Center is providing comes through its survivorship program, which helps patients deal with issues that arise after their cancer treatment has concluded.
“With more than 15 million cancer survivors alive in the U.S. today, we have an obligation to make sure that we’re also staying with those patients and making sure they’re dealing with whatever issues are associated with their survivorship,” Carte said.
Melissa Bedilion, RN, oversees the survivorship program, which helps patients with the lingering issues of having cancer, such as depression, financial issues, long-term side effects of their treatment and follow-up appointments.
“The survivorship program is kind of a new thing we just started last year,” Bedilion said. “When a patient finishes their treatment, navigators assist me in coming up with a survivorship care plan, so we can review that with the patients. It talks about prolonged side effects that might go along with their treatment, such as numbness or tingling that might require medication. There’s a formatted follow-up schedule that shows how often they’re going to see the doctor over the next five years, as well as any lab tests or X-rays they might need, information about any side effects they had during treatment and more. All of the doctors involved get a copy of the plan as well.”
As for the future of cancer treatment itself, Carte said much of the focus of current research is on immunotherapy, which is a treatment method that helps to enable the body to recognize cancer cells as harmful and fight them itself.
“Immunotherapy is really being researched extensively and has been added to a lot of different treatment regimens,” Carte said. “Immunotherapy enhances some of the already internal processes that allow us to fight cancer more effectively. It’s one of the ways that they’re looking to make sure that it works on a cellular level within the body, so that whatever’s going on with those cells, it actually addresses that specifically. It is those types of medications that I think over the last year has inundated cancer care, and it is important for cancer centers to keep up with the most updated treatment modalities. That’s something that I think we have really focused on here — making sure that we always have that available to our patients, as well as our physicians.”
WVU Medicine is working to provide top quality cancer treatment not only to the Morgantown area, but in different locations around the state.
Dr. Hannah Hazard, director of clinical services for the Mary Babb Randolph Cancer Center and WVU Cancer Institute, said the Institute is working with several regional providers to bring up-to-date cancer treatment closer to their patients.
“Over the last 18 months, we have incorporated our cancer practice in several other sites across the region,” Hazard said. “The intent is to allow patients to stay closer to home for a lot of their clinical care. Once a patient reaches a level of clinical stability that can then be managed at home, we want to be able to send these patients locally to their community. Most patients’ support comes from their family and their community, so having to travel hours to us on a regular basis for something they can achieve at home is counterproductive. It makes more sense for them to stay at home so they can have their support system.”
Hazard said the Institute is working to develop clinics in Parkersburg, Martinsburg, Elkins, Garrett County, Maryland and the Northern Panhandle.
“We also try to streamline the process for our new patients so they can see every specialist they need to on their initial visit,” Hazard said. “There’s a lot of moving parts involved there that you need to happen all at the same time, so we’re always striving to make that process easier and more convenient.”
Dr. Richard Goldberg, director of the WVU Cancer Institute, said cancer treatment is constantly changing, but that immunotherapy has been a large focus over the past year.
“The American Society of Clinical Oncology released a brochure on the biggest advances in cancer for 2016, and it was all immunotherapy,” Goldberg said. “Just recently, there has been a whole new class of drugs found called PD1 inhibitors that essentially take the mask off the cancer cells and let the immune system recognize them for what they are. We’re seeing what I would consider almost magical responses in some patients. They talk in medicine about what’s called the Lazarus effect — Lazarus rose from the dead — which I had never observed until using this immunotherapy in patients with colorectal cancer. I have this amazing young woman who was a dancer and had an inherited form of colon cancer. She came to me in a wheelchair and could barely hold her head up, but after four doses of the drug, she was back to professional dancing. That’s just not something we ever saw before, so these PD1 inhibitors are really the emphasis of many different pharmaceutical companies.”
Goldberg said other treatment options have also seen advances.
“Robotic surgery is becoming more and more common,” Goldberg said. “And in radiation, we’re seeing what’s called intensity modulated radiation, where doctors very carefully map out the tumor and attempt to hit it from multiple directions while sparing the adjacent healthy tissue. One of the problems with radiation is it eradicates tumors, but it doesn’t differentiate tumor tissue, so it damages everything in its path. The newer computer simulations associated with intensity modulated radiation can help to minimize that.”


























Post a comment as Anonymous Commenter
Report
Watch this discussion.
(0) comments
Welcome to the discussion.
Log In
Keep it Clean. Please avoid obscene, vulgar, lewd, racist or sexually-oriented language.
PLEASE TURN OFF YOUR CAPS LOCK.
Don't Threaten. Threats of harming another person will not be tolerated.
Be Truthful. Don't knowingly lie about anyone or anything.
Be Nice. No racism, sexism or any sort of -ism that is degrading to another person.
Be Proactive. Use the 'Report' link on each comment to let us know of abusive posts.
Share with Us. We'd love to hear eyewitness accounts, the history behind an article.